The management of severe burns is clearly a challenge, not only acutely but also from the standpoint of reconstruction and rehabilitation. Burn victims, especially children, with visible scarring and other resultant deformities have significant changes in self-esteem, happiness, and satisfaction. Therefore, whatever we can do to improve their appearance is extremely important and rewarding.
The reconstruction of burn alopecia thus far has been done primarily by the use of hair plugs, scalp flaps, free scalp flaps, and tissue expansion. Hair plugs require multiple procedures and tend to look artificial (cornfield rows, clumps of hair).1 Scalp flaps can be an excellent choice in certain cases, but scarring may be a problem.2,3 Free scalp flaps can certainly provide superb results in selected cases, but they require microvascular anastomosis, with its accompanying difficulties and complications.4 Tissue expansion has been the most popular way to reconstruct the burned scalp. It has produced satisfactory results, although it requires several procedures and sometimes repeated expansions. 5-7
We traditionally tend to think that grafts do not thrive well on grafts, especially in burned or scarred areas. However, having seen the survival of micrografts and minigrafts in patients with scarred scalps from various techniques used for the treatment of male pattern baldness,8-11 I felt it was worthwhile to try them in patients with burn alopecia.
Because the micrografts (one or two hairs) and minigrafts (three to four hairs) are so small, they have a lesser metabolic requirement for survival than larger grafts. It is encouraging to see that even when they are as close as 1.5 to 2 mm from each other, they still have an excellent survival rate.
Technique
As previously described for the treatment of male pattern baldness,8-11 intravenous sedation is accomplished by using Versed (midazolam), Sublimaze and local anesthesia consisting of 0.5% Marcaine (bupivacaine) with 1:200,000 epinephrine. Occipital nerve blocks are then done to harvest a horizontal donor strip, ideally from the occipital area, unless this is not available. The donor site is undermined and closed primarily with 3-0 Prolene sutures.
The micrografts and minigrafts; are dissected carefully, and the recipient site is then prepared by injecting it with tumescent solution (consisting of 0.25 Xylocaine with 1:200,000 epinephrine) for purposes of hemostasis and temporarily thickening the area to be grafted. This facilitates the insertion of the grafts.
The recipient sites are created by making slits with a 65 Beaver miniblade or a Feather 11 blade, and the grafts are inserted with a pair of jeweler’s forceps without the use of dilators. A special effort is made to create the slits and insert the grafts in the direction of the desired (natural) hair growth.
For dressing, we use Adaptic, wet Kerlix (in normal saline), dry Kerlix, and an Ace (elastic) bandage for 48 hours, after which the patient is allowed to shampoo gently. The sutures from the donor site are removed at 7 to 10 days postoperatively.
The grafts grow hair immediately for the first 10 to 15 days, after which most of it is shed (telogen), but about 95 percent of the grafts regrow the hair at 3 to 4 months postoperatively (anagen). It takes about 6 months for the hair to look good, and about 10 to 12 months for the final result.
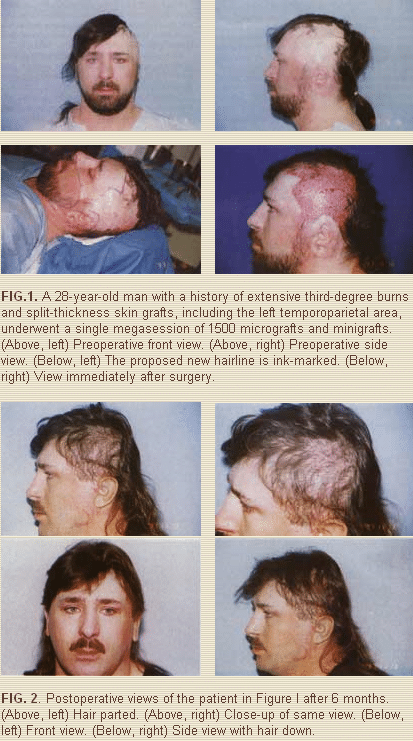
Case 1
A 28-year-old man was burned with hot tar on his upper body, neck, face, and scalp and also lost his left ear. He had extensive, multiple, split-thickness skin grafts, including the left temporoparietal area. He refused the use of tissue expansion and was treated by a single megasession of 1500 micrografts and minigrafts (Fig. 1). The result shown in Figure 2 is after only 6 months. Subsequently, he underwent a second procedure to further increase the density of hair. He had no complications.
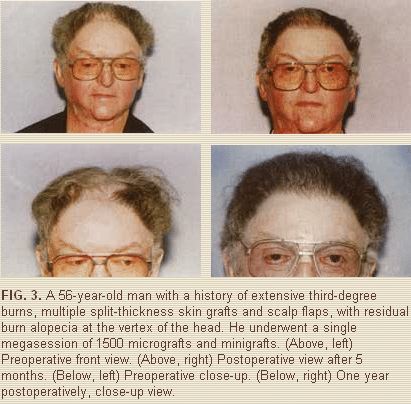
Case 2
A 56-year-old man was in an explosion and burned with propane vapors. He had extensive burns and barely survived. He had multiple surgical procedures, including skin grafts and scalp flaps, Figure 3 shows him at both 5 months and I year after a single megasession of 1500 micrografts and minigrafts to the entire vertex of the head. He had no complications.
Discussion
Each case must be evaluated individually to determine if the patient is a candidate for micrografting and minigrafting or for another technique. The areas of burn alopecia should be in relatively good condition, that is, they should have some thickness and pliability and the scar tissue should have somewhat matured. We have learned that micrografts and minigrafts thrive well, even in areas of precarious blood supply, such as areas of third-degree burns and areas that were split-thickness skin grafted, as shown in the cases presented. In cases where the area to be reconstructed is excessively fibrotic and extremely thin, tissue expansion or scalp flaps may be a better choice.
There is no technique today that will create new hair per se (new hair follicles); what we are doing with the use of micrografts and minigrafts or with any other technique is a redistribution of the patient’s own existing hair. Obviously, the patient must have a good donor area and a favorable ratio of the area to be reconstructed (hopefully small), to the donor area (hopefully large).
Preferably, the area to be reconstructed should be less than 50 percent of the total scalp surface, and the remaining donor scalp ideally should be densely populated with hair genetically programmed to stay. In other words, you do not want to harvest from the crown on a young man who may lose his hair as he develops male pattern baldness a few years later. In such a case, you only want to harvest from the occipital area, as we normally would for cases of male pattern baldness, if it is available.
Clearly, the greater the area to be reconstructed in relation to the size and quality of the donor area, the less ideal the candidate becomes. This applies to any and all techniques.
As in cases of male pattern baldness, if the ratio is not favorable, one must concentrate on areas of greater importance first, such as the front hairline, and the most anterior areas, such as temporal areas and the sideburns. The cases presented were favorable candidates; both later underwent a second megasession to further increase hair density. As long as good and dense donor areas exist, the procedure can be repeated up to three or four times, when feasible. Most patients who have this technique of hair transplantation, however, undergo only one or two sessions.
Summary
The treatment of burn alopecia is a very challenging problem. Several techniques have been described in the past, mainly punch grafts, local scalp flaps, free scalp flaps, and tissue expansion.
The fibrotic scar tissue that normally results after burn injuries has a precarious blood supply and is not an optimal ground for any type of graft. Single and double hair grafts (micrografts), and grafts with three to four hairs (minigrafts), because of their small size, have less metabolic requirements and are able to survive and grow healthy hair, even under adverse circumstances. Having seen these small grafts survive in scarred scalps from previous surgical procedures while treating patients with male pattern baldness, I believed it would be worthwhile to try them in cases of burn alopecia.
The procedure is performed under mild intravenous sedation and local anesthesia in our operating room suite. Two cases are presented to illustrate the results that can be obtained with micrografts and minigrafts in a single session. They confirm that these small grafts survive, even over third-degree burn areas that have been split-thickness skin grafted, and that the grafts are safe and provide a natural result.
Alfonso Barrera, M.D.
West Houston Plastic Surgery Clinic, P.A.
915 Gessner Rd., Suite 825
Houston, TX 77024
